Round Table Discussion with RMIG
Cherie Bragg, Performance Improvement Coordinator, Recall Administrator, Six Sigma Black Belt, Corporate Supply Chain, Yale New Haven Health
Emily Funk, Project Coordinator, Yale New Haven Health
Anna Cerilli, Value and Safety Clinical Coordinator, Corporate Supply Chain, Yale New Haven Health
Jennifer Sanders, Contract Portfolio Manager, Froedtert Health
Mandy Peters, Informatics Analysis with Focus on Recalls, Froedtert Health
Amy Conway, Enterprise Recall Analyst, Supply Chain Management, Mayo Clinic
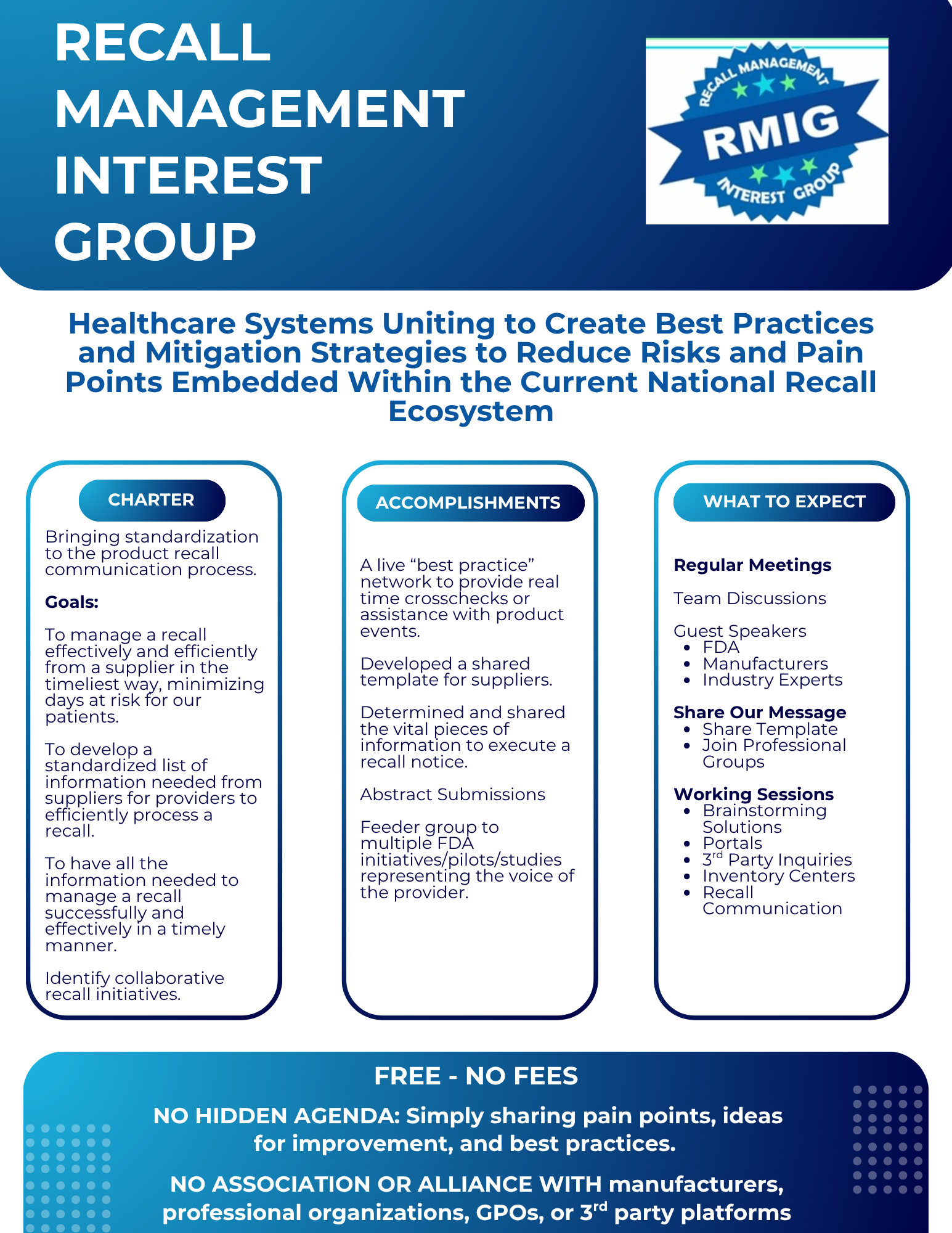
Recall management is a challenging area for healthcare organizations throughout the country as there is no set methodology, workflows, standardized tools, or training. Healthcare organizations are now developing their own recall management processes, workflows, and problem-solving tools. Luckily, a group of large health systems have gotten together to form the Recall Management Interest Group (RMIG) to help solve all the issues surrounding recall management and create best practices. This round table interview discussion today is with three Healthcare System Recall Management Leaders who are taking this challenging area to task and solving the challenges that have turned RMIG into a major positive force for advancing recall management in our industry.
HVAUMM: I think it is important for us to start with the definition of what recall management truly is in 2025 and beyond. Could you share what your definition is?
JS & MP – Froedtert: Recall management today is an intricate ecosystem that spans a vast and dynamic network — from the FDA and manufacturers to distributors, healthcare systems, and ultimately, patients. The core objective remains constant: speed to safety, with patient well-being always at the forefront.
CB, EF, & AC – YNHHS: We affectionately call recall management in its current state, “The Wild West on the verge of enlightenment.”
“Recalls” encompass all manufacturer safety notifications, from lightbulbs to heart valves, regardless of whether they involve product removal or not. This includes manufacturer instructions for use (MIFU) updates, field corrective actions, recall/removal of product, manufacturer safety bulletins, and others.
Recall management in healthcare systems incorporates the full life cycle of the notification, from receiving, taking action, internal communication, removal if applicable, risk management, documentation, and external closure.
Wild West (current) = everyone is following their own processes (manufacturers, distributors, and providers)
Enlightenment (beyond) = working toward standardization
AC – Mayo: It means we’ve finally admitted that recalls are not just about pulling faulty devices — they’re about managing chaos across an entire health system in real time.
In 2025, recall management covers every kind of manufacturer notification: product removals, field corrections, safety bulletins, MIFU updates — you name it. And let’s not forget, the FDA labels everything a “recall”. But if it affects patient safety or how we’re supposed to use something, it’s on our radar.
Managing recalls is not a single event. It’s a full-cycle operation. From the second that notice hits your inbox, you’re assessing risk, chasing down products, alerting clinical teams, relying on the value analysis team, and coordinating with procurement and inventory teams to secure clinically approved substitutions — often while navigating back orders, stock outs, and allocations, while also documenting every move and proving compliance — usually with incomplete info, inconsistent formats, and zero automation.
The difference now is that health systems are waking up to the fact that this isn’t just a back-office admin task. It’s clinical. It’s operational. It’s legal. And it needs a system — one that’s scalable, standardized, and doesn’t rely on heroic effort every time.
HVAUMM: How did Recall Management Interest Group (RMIG) come together?
AC – Mayo: RMIG started as a bit of a group therapy session. A few of us — Mayo, Yale New Haven, Froedtert — started checking in with each other like, “Are you seeing this mess, too?” We were all getting buried in recalls, trying to make sense of supplier portals that felt more like escape rooms, and suppliers kept telling us, “Other hospitals love our process.”
And quite quickly, we realized we weren’t the problem, the recall system as a whole was broken. From there, things snowballed. We started meeting regularly, swapped best practices, built out templates, and before we knew it, more hospitals were asking to join. We began to share our visions at conferences and doubled our membership in less than a month.
Turns out, we’d accidentally started a national movement. RMIG was born from chaos, a shared drive to do better, and a network of strong, smart, sassy women determined to stop fixing the same mess alone — and start fixing it together.
JS & MP – Froedtert: The Recall Coordinator role can often feel isolated within health systems. Through networking, we realized that many of us were working in parallel rather than in unison — each tackling similar challenges without the benefit of shared strategies or collaboration.
CB, EF, & AC – YNHHS: Mayo, Yale, and Froedtert had been leaning on each other as resources, often meeting informally about recalls. When supplier portals began emerging, it created confusion and operational friction. We reached out to one another to compare how our systems were responding. The more we talked, the more we realized a shared voice could be powerful in advocating for changes and raising concerns with suppliers. We also wanted to know — were other health systems experiencing the same challenges?
Suppliers would often tell us, “Other systems love our portals,” implying we were the outliers. But by connecting, we learned we weren’t alone. Regular meetings followed where we shared best practices, collaborated, and brainstormed solutions. The group grew quickly once word got out. It became clear there was a real industry need for this kind of collaboration.
HVAUMM: Why does recall management create such problems for health systems today even though there is a high level of technology available to health systems throughout the country?
JS & MP – Froedtert: Within healthcare systems, there’s often such a strong focus on clinical advancements that clerical and operational improvements can fall behind. Recall management is a prime example — many of us have identified it as an area still relying on what feels like ‘archaic’ technology.
Even after establishing centralized communication processes — like a single recall email inbox (e.g., fhrecalls@froedtert.com) — we continue to receive recall notices via snail mail. This points to a broader issue in the ecosystem.
By centralizing communication through supply chain teams, we’ve created a unified communication template that ensures clinical teams receive the same information, at the same time, with the same expectations. This approach helps prevent the “wildfire effect” — where inconsistent messages cause confusion and delays across departments.
Through RMIG, we’ve observed that many external solutions are still being developed in silos — often without the involvement of key stakeholders, such as healthcare supply chain subject matter experts. Bringing the right voices to the table is essential for creating sustainable, effective recall management strategies.
AC – Mayo: None of the technology is pointed at the problems like having a clear standardized communication delivered as an email to the required recall inbox.
Health systems have million-dollar surgical robots and AI that read radiology scans — but when a recall hits, we’re still chasing PDFs, digging through supply closets, and relying on email chains that start in legal, bounce through risk, loop in leadership, make a pit stop with nurse managers and patient safety — and finally, eventually, end up in my inbox.
The core issue? Vendors don’t all follow the same rules. Notices come in at random times, through different channels, with different formats, and constant inconsistent detail. Sometimes it’s a formal letter. Sometimes it’s a three-line email. Sometimes it’s…a fax.
Even when we try to digitize the process, it usually means logging into a portal, clicking through eight tabs, downloading a PDF, and pretending that counts as streamlined. We require digital communication, but it’s more like digital-ish. And yet, electronic communication for recalls has been FDA-approved since 2006 — yeah – 2006, almost 20 years ago!
That’s why RMIG is stepping in. We’re not waiting around for someone to save us. We’re creating the standards, the templates, and the shared voice to fix this from the inside out.
|
A Day in the Life of a Recall
But then… We receive a similar (but slightly different) notice from a distributor. Then a third notice from a second distributor. Each one potentially contains new information — added part numbers, conflicting messaging — requiring repeated sweeps. Every notice must be re-evaluated. Without standardization, even a slight change may have major implications. What looks like a duplicate may actually be a crucial update. |
CB, EF, & AC – YNHHS: Even though technology has advanced, there is no universal or perfect system — and no standardization across platforms. Some recall systems are supplier-focused; others are designed for health systems. Yet none bridge the two effectively. Many suppliers still rely on outdated methods like snail mail, even though email has been FDA-approved since 2006.
RMIG created the motto “Speed to Safety” to capture our goal: To receive a notification and act on it quickly to protect patients. But due to the lack of standardization, a process that should take one day often stretches to 45 days or longer.
HVAUMM: What are some of the biggest obstacles you face with recall management at your health system?
JS & MP – Froedtert: The lack of external standardization in required fields creates significant roadblocks when attempting to release recall notices effectively. Without standardized communication templates, delivery methods, or reply protocols, the process becomes fragmented. Additionally, the data being sent in indigestible formats leads to time delays and increases the potential for human error, making an already complex process even more prone to mistakes.
AC – Mayo: Getting the right information to the right recall contact within every hospital fast enough to protect patients.
Every recall is a race — a race that was unannounced, and instead of a starting gun, someone just handed us a marathon vest mid-sprint and told us to run. Sometimes we’re well into the distribution process before details surface that make us pause and triple-check whether something is affected — usually while juggling six other moving parts and trying not to clog anyone’s inbox in the process. And that’s not because we’re disorganized. It’s because the information we need is often incomplete, buried in legalese, sent to the wrong person, or filtered through five vendor systems before it reaches the front line.
We call our approach Speed to Safety for a reason. The end game isn’t paperwork. It’s preventing patient harm. But when you spend the first 48 hours just trying to understand what the manufacturer is actually asking you to do (in a document marked URGENT), you’re already behind.
HVAUMM: Why Is RMIG so important when every health system operates differently?
JS & MP – Froedtert: Having the opportunity to network with others doing the same work has been invaluable in driving best practices. On average, we’ve found that health systems typically dedicate just 1.25 FTEs to recalls — which can make the role feel isolating and overwhelming. Through collaboration, we’ve built a community that not only shares knowledge but also supports one another in pushing the work forward. It’s the kind of progress that would be hard to achieve alone.
CB, EF, & AC – YNHHS: Three factors: A unified voice that we now speak to suppliers and stakeholders with shared concerns and priorities. Shared knowledge, even though systems are different, the problems are often the same. Common goals – it is patient safety, efficiency, and reducing the burden on staff that unites us.
AC – Mayo: No two health systems are alike — supply chain structures vary, clinical workflows are customized, and recall processes range from fully centralized to, “Angela in Sterile Processing just handles it.” And yet, we’re all being asked to respond to the same manufacturer notices with the same urgency, using tools that were clearly built without us in mind.
|
Why RMIG Matters RMIG gives us a shared brain – a place to compare notes, test ideas, and build the kind of practical tools we all wish had existed years ago. It’s not about making every hospital operate identically. It’s about giving providers a collective voice to define what good looks like. It’s about standardizing what can be standardized — like templates, communication formats, and expectations — so we can respond faster and smarter, no matter how our charts are shaped. RMIG has become a go-to resource – something we rely on regularly, not just when things go wrong. It’s where we turn for real-world tools, vetted solutions, and collective insights. Whether it’s a shared SOP, a recall notice template, or a group text to sanity-check a vendor’s latest portal stunt — RMIG helps us actually get stuff done. |
HVAUMM: How are health systems training people in recall best practices?
CB, EF, & AC – YNHHS:
- There is not a standard for best practices or training
- Every health system is different
- Their stage of their recall management program (if they have one) and the staff that support it. Not all are in VA or Supply Chain
- FTE
- YNHHS has a comprehensive training program for all recall-facing staff
- The health system has a recall management policy
- KPIs reported out monthly to leadership and front-line staff
JS & MP – Froedtert: While there isn’t a formal training program in place for staff, our dedicated recall email inbox has helped increase awareness across the system. By including policy references and relevant resources at the end of every communication, we’re able to provide ongoing education in real-time, embedded directly within the process.
AC – Mayo: Most people involved in recalls were never trained in recalls. They were voluntold, looped in mid-crisis, or just happened to be the one who responded to the first email. There’s no onboarding for ‘here’s what to do when a critical device gets recalled and there’s no replacement available — oh, and surgeries are scheduled in 20 minutes.’ And don’t get me started on the confusion around “voluntary” recalls — where folks assume it’s optional to remove a dangerous device, when in reality it just means the manufacturer issued it without an FDA mandate. It’s voluntary for them to initiate, not for us to act.
That’s why RMIG is working on recall-specific education that acknowledges the clinical and supply chain perspective.
HVAUMM: Where is recall management going with RMIG leading the way?
CB, EF, & AC – YNHHS:
- Create processes that build trust within the recall ecosystem (all stakeholders, providers, users, suppliers)
- Addressing issues identified in question 4.
- This will facilitate buy-in from leadership across all organizations and industries (providers & suppliers)
AC – Mayo: With RMIG, we’re not just reacting anymore. We’re shaping the future of how recalls are handled in healthcare — standardizing processes, defining expectations, and putting real pressure on manufacturers to deliver usable information the first time. And we’re doing it with the collective voice of over one hundred health systems across the nation behind us.
And yes, that includes the cost recovery conversation.
For years, hospitals have eaten the cost of product failures, staff time, and supply chain disruption — while manufacturers offered little more than a blanket apology and a return label. That’s starting to change.
One of the loudest silences in recall management is reimbursement. Providers eat the cost of recalls while manufacturers walk away with clean hands and a new product line. If recalls are a two-way street, it’s time both parties split the toll.
“In most health care systems, Corporate Supply Chain is charged with the responsibility of managing recalls. Although the CSC teams are not bedside, we truly believe that our diligence with Speed to Safety and our handing of each recall with expertise and precision saves lives.” -Froedtert
For more information about the Recall Management Information Group (RMIG) please use the QR Code below:
Articles you may like: