In the ever-evolving landscape of healthcare, the integration of evidence-based practice (EBP) into the healthcare value analysis process is pivotal. EBP involves the conscientious use of current best evidence in making decisions about patient care, combining clinical expertise, patient values, and the best available research. Incorporating EBP into healthcare value analysis ensures that clinical decisions are grounded in solid scientific data, ultimately advancing patient care and optimizing resource utilization. EBP is a cultural commitment of a healthcare organization towards using data-driven approaches to improving quality and competent care. This also requires engagement from clinicians, healthcare leaders, and industry partners in parallel to advance this critical mission.
The Significance of Evidence-Based Practice
Evidence-based practice is essential for several reasons:
- Improved Patient Outcomes: By basing clinical decisions on the most reliable evidence, healthcare providers can enhance patient outcomes. Treatments and interventions supported by high-quality evidence are more likely to be effective and safe.
- Cost-Effectiveness: EBP helps identify the most efficient and cost-effective treatments, reducing unnecessary spending on ineffective or harmful interventions. This is critical in an era of rising healthcare costs.
- Standardization of Care: Implementing EBP promotes standardization across healthcare settings, reducing variability in care delivery and ensuring that all patients receive the best possible care based on current research.
- Patient Satisfaction: Patients are more likely to trust and adhere to treatment plans that are backed by scientific evidence, leading to higher satisfaction and better overall health outcomes.
Levels of Scientific Evidence
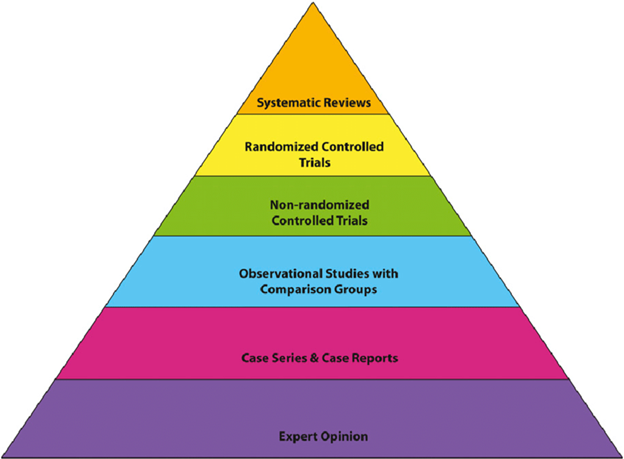
Understanding the different levels of scientific evidence is crucial for effectively incorporating EBP into the healthcare value analysis process. These levels, often depicted in a hierarchy, help determine the strength and reliability of the evidence.
- Level I: Systematic Reviews and Meta-Analyses of Randomized Controlled Trials (RCTs)
- These provide the highest level of evidence as they synthesize data from multiple RCTs, offering comprehensive insights into the effectiveness of interventions.
- Example: A meta-analysis of multiple RCTs on the efficacy of a new drug for treating hypertension.
- Level II: Randomized Controlled Trials (RCTs)
- RCTs are considered the gold standard for testing the efficacy of interventions due to their rigorous design, which minimizes bias.
- Example: An RCT comparing the outcomes of two different surgical techniques for knee replacement.
- Level III: Controlled Cohort Studies
- These studies follow groups of patients over time and compare outcomes between those who received the intervention and those who did not.
- Example: A cohort study examining the long-term effects of a dietary intervention on diabetes management.
- Level IV: Case-Control Studies
- These studies compare patients with a particular condition (cases) to those without the condition (controls), looking back retrospectively to identify possible causes or risk factors.
- Example: A case-control study investigating the association between smoking and lung cancer.
- Level V: Case Series and Case Reports
- These involve detailed reports on a single patient or a small group of patients, providing insights but with a lower level of evidence due to lack of control groups.
- Example: A case series describing the outcomes of patients treated with a new type of wound dressing.
- Level VI: Expert Opinion
- Expert opinion is the lowest level of evidence, relying on the clinical expertise and experience of healthcare professionals.
- Example: Clinical guidelines developed based on expert consensus when higher levels of evidence are lacking.
*Image used with permission from Researchgate
Leveraging Evidence-Based Practice in Healthcare Value Analysis
Integrating EBP into the healthcare value analysis process involves several steps:
- Literature Review and Evidence Gathering:
- Conduct comprehensive literature reviews to gather the best available evidence related to the healthcare products, technologies, or interventions under consideration.
- Utilize databases such as PubMed, Cochrane Library, and Embase to access high-quality research studies and systematic reviews.
- Critical Appraisal:
- Critically appraise the gathered evidence to assess its validity, reliability, and applicability to the specific healthcare context. Tools like the Critical Appraisal Skills Programmed (CASP) checklists can assist in this process.
- Evaluate the methodology, sample size, and potential biases in the studies to ensure robust decision-making.
- Integration with Clinical Expertise and Patient Preferences:
- Combine the appraised evidence with clinical expertise and patient preferences to make informed decisions. This holistic approach ensures that the chosen interventions align with the clinical context and individual patient needs.
- Engage multidisciplinary teams, including clinicians, nurses, and pharmacists, in the decision-making process to incorporate diverse perspectives.
- Implementation and Monitoring:
- Implement the selected interventions and monitor their outcomes continuously. Use performance metrics and patient feedback to assess the effectiveness of the interventions and make necessary adjustments.
- Foster a culture of continuous learning and improvement, encouraging healthcare teams to stay updated with the latest research and integrate new evidence into practice.
- Education and Training:
- Provide ongoing education and training to healthcare professionals on EBP principles and techniques. This can include workshops, seminars, and online courses.
- Equip healthcare teams with the skills to critically appraise research and apply evidence in their clinical practice.
Incorporating evidence-based practice into the healthcare value analysis process is essential for advancing patient care, improving outcomes, and optimizing resource utilization. By understanding the different levels of scientific evidence and leveraging them effectively, healthcare organizations can make informed decisions that enhance the quality and efficiency of care delivery. Embracing EBP not only benefits patients but also empowers healthcare professionals to provide the best possible care based on the most reliable evidence available. As the healthcare landscape continues to evolve, the commitment to evidence-based practice will remain a cornerstone of high-quality, patient-centered care.
Article By:
Hudson Garrett Jr., Ph.D., MSN, MPH, MBA, FNP-BC, IP-BC, PLNC, VA-BC, BC-MSLcert™, MSL-BC, CPHRM, LTC-CIP, CPPS, CPHQ, CVAHPTM, CMRP, CPXP, CDIPC, FACDONA, FAAPM, FNAP, FACHE, FSHEA, FIDSA
Dr. Garrett is the Executive Director and Executive Vice President for the Association of Healthcare Value Analysis Professionals (AHVAP) and an Adjunct Assistant Professor of Medicine in the Division of Infectious Diseases at the University of Louisville School of Medicine.
Karen Niven, MS, BSN, RN, CVAHPTM
Karen Niven is the Senior Director of Clinical Value Analysis at Premier, Inc. and serves as the President-Elect for the Association of Healthcare Value Analysis Professionals (AHVAP).
Articles you may like:
Establishing a Pathway to Professional Accountability for the Specialty of Healthcare Value Analysis