Erica DeBoer, MA, RN, CCRN-K, Sanford Health
Kimberly Alsbrooks, BSN, RN, RT (R), VA-BC, BD
Halit O. Yapici, MD, MBA, MPH, Boston Strategic Partners
Importance of Urinary Catheter Management and Supply Chain Process
According to the Centers for Disease Control and Prevention (CDC), 12% to 16% of adult hospital inpatients receive indwelling urinary catheters, which makes it one of the most commonly used medical devices in the hospital setting.1,2 Each additional day with an indwelling urinary catheter may increase the chance of catheter-associated urinary tract infections (CAUTI) by 3% to 7%,2 which is likely associated with over $1,000 in costs per event (up to $10,197 for Intensive Care Unit [ICU] patients) adding to a total US burden of $1.7 billion.3 Moreover, indwelling catheters may lead to several issues including catheter encrustation, leakage, and discomfort.1 An evidence-based approach to catheter insertion and management can reduce the rate of negative outcomes and related costs.1
The hospital supply chain is particularly complex since medical supplies often go through several steps (i.e., processing by central stores prior to delivery to end-user) before being available at multiple clinical departments for patient-care.4 Furthermore, clinical staff contributes to supply chain/logistics activities which means almost everyone is involved in the supply chain.4 In fact, over 10% of the clinical staff time and 40% of hospital expenses are spent on supply chain activities.4 Therefore, effective supply chain management initiatives not only reduce costs but also lead to improved quality of care and job satisfaction among clinical staff.4 A lack of communication between manufacturers and materials managers, fragmented supplier base (i.e., a large number of vendors), and non-standard purchasing processes are key issues in hospital supply chain management.5
Participation from a wide range of internal and external stakeholders, and collaborative planning is necessary to address key issues outlined above.5,6 An interdisciplinary improvement team representing medicine, nursing and administration should be involved since “the people who do the work need to be the ones to change the work”.7 Engagement of clinicians is especially crucial because they can provide knowledge and perspectives which can significantly contribute to success.7
 About Sanford Health
About Sanford Health
Sanford Health is one of the largest health systems in the United States. After its merger with the Evangelical Lutheran Good Samaritan Society in 2018, Sanford delivers integrated healthcare, genomic medicine, senior care and services with 44 hospitals and 482 clinics spanning 26 states and 9 countries. Sanford’s organizational structure consists of four major regions, including its headquarters in Sioux Falls, SD as well as three regional offices in Fargo, ND, Bismarck, ND, and Bemidji, MN.8
The Impetus for Change
In 2016, Sanford recognized the need for a consistent urology catheter management policy across its network. The goal was to reduce variation in patient care and increase supply chain efficiency by standardizing policies and products across the organization. Sanford’s leadership understood the value of collaborative planning for the long-term success and sustainability of the initiative and partnered with BD. A wide range of expert clinicians from Sanford were also involved in the planning and implementation of the initiative specializing in infection control, education, quality, and supply chain teams as well as physician leadership. Additionally, project champions from Sanford Health were selected in each nursing unit from the frontline clinical staff to support the implementation.
Before 2016, urology catheters at Sanford Health were stocked based on local value analysis and products differed within and across care settings. Hundreds of different products were carried by medical centers causing inefficiencies in ordering, stocking, troubleshooting backorders, and dealing with product expiration. Furthermore, nurses often had to “mix and match” these products to prepare them for clinical use, taking time away from patient-care activities. 9 Significant resources were being spent on training the clinical staff in using a variety of products appropriately. Previous attempts to standardize the catheter management process and reduce associated supply chain waste were limited to local initiatives focusing on managing stock-keeping units (SKUs) and revising urology catheter policies.
The 2016 Initiative at a Glance
Sanford adopted a data-driven, evidence-based, and clinically-led strategy to identify and address the gaps in the catheter management process. First, each product went through a comprehensive evaluation based on specific criteria, including its impact on patient care and ease of use. Only the items that provide the highest overall benefit to patients were maintained in the system, while others were eliminated from the ordering list. As a result, Sanford decreased the number of line items in purchase orders by 74% and decreased the number of vendors to one.9 The economic benefits of reducing the number of suppliers, establishing standard order management processes, and minimizing SKUs are well-documented in the literature.5
The catheter management initiative at Sanford was not limited to efficiency improvements in the supply chain. To ensure excellence in patient-care, Foley kits and post-insertion wipes were made available in every single unit. These easy-to-use kits include everything that a nurse may need to complete a sterile catheter insertion, including step-by-step directions. Specific patient needs were also prioritized as coudé tip catheters became a standard for the adult male patients and modified Foley kits for patient subpopulations (i.e., patients with allergy to latex products) were made available in every unit.
Planning for the Hurdles
The implementation was not without challenges. The full implementation of the initial changes took around a year including the planning phase. Evaluating hundreds of products in terms of benefits to patient care was especially time-intensive. An evidence-based approach and clear criteria allowed Sanford to complete this process without delays. Moreover, Sanford often used the ICU as a pilot before expanding the processes to the enterprise since ICU had the highest catheter utilization. Lessons learned from the smaller scale ICU implementation allowed Sanford to achieve a smooth transition across the enterprise.
An extensive communication and education strategy complemented the implementation process to prevent any challenges regarding stakeholder buy-in. Effective and open communication was achieved through close coordination at the enterprise and regional levels. Hands-on product training and education, classroom sessions, and training materials were provided to ensure the appropriate use of the available urology catheter products. In-person and teleconference meetings and email communications were used to disseminate the benefits and rationale behind the new catheter management processes and to receive feedback. The project team addressed questions and concerns from the stakeholders by providing examples from the literature and data from the early improvements at Sanford which made these communications especially effective in convincing various stakeholders.
Continuous Improvement
Aiming for absolute excellence in patient care, Sanford Health continued to improve catheter insertion and management processes. Since the implementation of initial changes in 2016, Sanford health has adopted two-person urology catheter insertion and made external catheters available for both male and female patients.
Two-person insertion of urinary catheters allows one nurse to fully focus on ensuring the correct steps are followed while her/his colleague is cleaning the periurethral area of the patient and inserting the catheter. In this method, the second nurse reads step-by-step directions, observes the patient (i.e., look at the skin condition to decide the best catheter to use) and ensures sterile insertion. If the sterile technique is broken for any reason, the second nurse can stop the procedure. When necessary, the second nurse also supports her/his colleague in cleaning and positioning the patient, especially for patients with unilateral weakness, mental status changes, or post-operative pain. A significant reduction in CAUTIs following two-person catheter insertion is documented in the literature.10-12
Sanford Health also introduced external catheters to improve patient care and staff satisfaction. Using external catheters when feasible may be an effective strategy to minimize the utilization of indwelling catheters.13 Sanford Health used a trial method to decide the most appropriate external catheter to carry in its inventory. In the trial period, clinical units received several products as well as a scorecard to rate the products on a variety of criteria including easiness of use and patient satisfaction. Based on the results of the overall scores, Sanford decided on a male and a female external catheter. Nurses from varying regions and departments all expressed positive experiences and very high satisfaction with using external catheters; they wanted to see an increased use of these catheters in the future.9
Sustained Success
Following a successful implementation, sustainability is the main challenge. According to a systematic literature review, the median follow-up time after quality improvement interventions is less than 1-year.14 Reverting to prior practice leads to resource waste and may increase the resistance to future initiatives to improve patient-care15 since achieving stakeholder buy-in is likely to be more difficult after unsuccessful attempts to change behavior. Sanford employed several methods to avoid reversion to prior practice:
1.Education
Continuous product training and education have been a key component of sustainability from the beginning. The goals of the continuous product training and education programs included refreshing skills of experienced Sanford employees as well as training new hires in delivering efficient and high-quality patient care. Sanford holds annual skills fairs where nurse educators go over the urology catheter insertion, maintenance, and removal processes in detail. These trainings created by Sanford are also incorporated in the new hire orientation, where the nurses complete computer-based and hands-on trainings and are expected to demonstrate competence in their preceptors’ presence. Additional unit-centered product training and education programs are also provided on an as needed basis where nurse educators visit a unit and observe the status quo, identify gaps, and address these gaps with further trainings.
2. Monitoring
Sanford has been using multiple reporting systems to make sure the new catheter management process is functioning as intended. Trends in direct and indirect indicators such as indwelling catheter days, catheter utilization, and the number of CAUTIs are closely watched by weekly and monthly reports. Furthermore, infection prevention and compliance departments conduct occasional audits. BD also provided product training and education, including assessing whether Sanford clinicians used BD products consistent with their instructions for use.
Monitoring the improvements is not limited to reporting. Catheter management at Sanford is ever-improving, which is in line with the organization’s aim to provide the absolute best patient care. Every single issue identified by the reports or audits automatically triggers a detailed root cause analysis led by the hospital’s leadership. After the investigation, appropriate changes are made in the process to prevent issues from recurring.
Nurse leaders also play a critical role in improving catheter management and sustaining the benefits. Nurse leaders in each unit conduct daily patient rounds with the department nurses and discuss the prognosis of patients with urology catheters. For each patient, the nursing team considers whether the catheter can be removed to help decrease the CAUTI risk factors. When the urology catheter is a necessity due to the patient’s condition, the team also reviews less invasive options such as external catheters. These rounds have been an excellent opportunity to raise awareness among nursing staff regarding best practices in urology catheter management, as well as product options that are available at Sanford Health such as external catheters.
4. Adherence Policy
Sanford also adopted administrative policies to ensure adherence to the best practices and to provide the highest quality patient care. The organization’s adherence policy dictates consequences for clinical staff who deviate from the best practices ranging from re-education and oral/written warning to prevention from providing urology catheter-related care in the future (i.e., insertion, management, and removal). One of the supply chain management nurses added, “We are not doing this to be punitive. Our goal is to do what is best for the patient.”
The Long-Term Benefits
“More confidence and less confusion” is how a nurse leader describes the current situation at Sanford Health.9 Nurses from a variety of departments and regions expressed very high satisfaction with the improvements at the organization. An infection prevention nurse added, “Standardizing the product and policy is making us a highly reliable organization.”9 Day-to-day work is also easier for Sanford Health nurses as they can simply “grab the kit and insert the catheter.”9 The improvement in nurse satisfaction is likely to improve quality of care since association between nurse satisfaction and patient satisfaction is well-documented in the literature.16-18
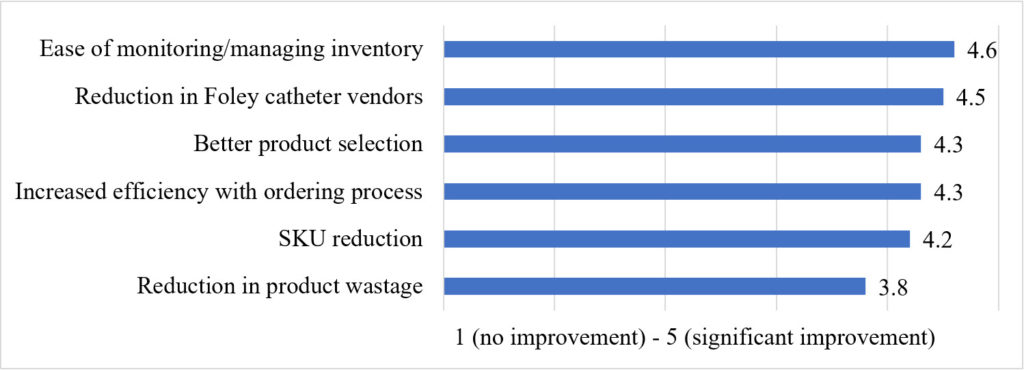
Sanford Health has sustained and improved the benefits of the catheter management initiative. Six months after the implementation, the formulary compliance among clinical staff increased from 35% to 95%.9 Nurses reported a decrease in indwelling catheter days and catheter utilization.9 Furthermore, they reported significant improvements in supply chain processes, including ease of monitoring and managing inventory. A summary of perceived supply chain-related improvements among nursing staff can be found in Figure 1.
Figure 1. Average Perceived Improvement (n=11)
The Right Partnership
BD’s partnership has been instrumental in the implementation and sustainability of the new catheter management at Sanford Health, and employees are highly satisfied with the partnership.9 BD prioritized Sanford’s goal in providing the highest quality patient care. According to the nurse leaders and other nursing staff at Sanford, BD’s attention to detail and responsiveness set it apart from the rest of the companies in the industry.
BD’s support consisted of:
- Conducting annual product trainings and education to show progress as well as areas for improvement
- Providing references through literature reviews to support Sanford’s evidence-based approach
- Supplying easy-to-use urology products (i.e., SureStepTM Foley Tray System)
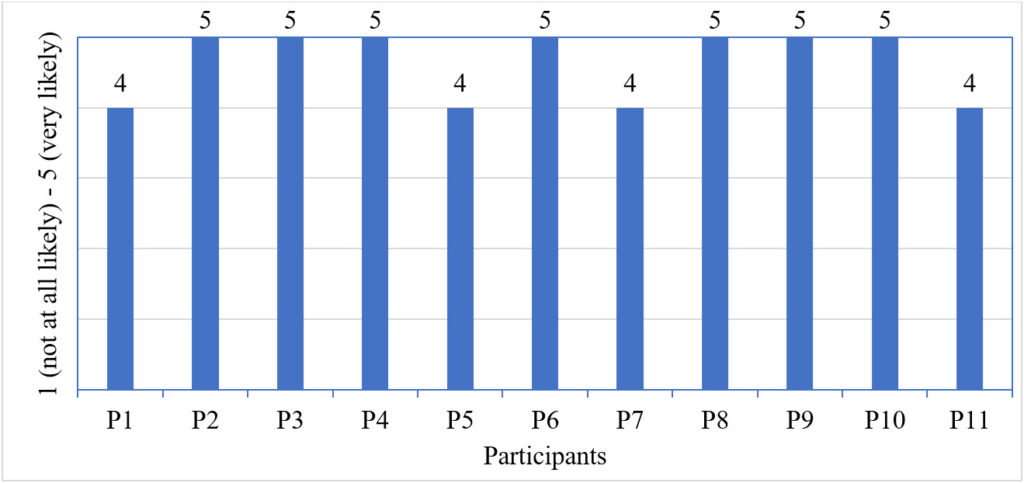
Sanford employees indicated that other health systems could also benefit from a similar catheter management initiative, especially the health systems that have a high variation across their care settings (i.e., health systems that recently went through a merger). However, several of the nurses underlined that a determined leadership and the right partnership would be necessary to replicate the success at Sanford Health.9 The likeliness of Sanford employees in recommending the initiative is illustrated in Figure 2.
Figure 2. The likeliness to recommend the initiative to other health systems (n=11)
This study demonstrates the value of standardization and quality improvement initiatives in the urology catheter management. With a strong leadership, internal/external stakeholder involvement, and an evidence-based approach, Sanford has successfully improved its catheter management process and realized significant clinical and economic benefits.
Correspondence:
Halit Onur Yapici,
Senior Consultant
Boston Strategic Partners, Inc.
4 Wellington Street Suite 3 Boston, MA 02118
Disclosure: This hospital experience report was sponsored by BD. Ms. Deboer is an employee of Sanford Health. Ms. Alsbrooks is an employee of BD. Dr. Yapici is an employee of Boston Strategic Partners Inc., contracted by BD to conduct the primary research and write the study.
References
- Smith JM. Indwelling catheter management: from habit-based to evidence-based practice. Ostomy/wound management. 2003;49(12):34-45.
- Centers for Disease Control Prevention. National Healthcare Safety Network (NHSN) Patient Safety Component Manual. In:2019.
- Hollenbeak CS, Schilling AL. The attributable cost of catheter-associated urinary tract infections in the United States: A systematic review. American Journal of Infection Control. 2018;46(7):751-757.
- Landry S, Beaulieu M. The Challenges of Hospital Supply Chain Management, from Central Stores to Nursing Units. In: Denton BT, ed. Handbook of Healthcare Operations Management: Methods and Applications. New York, NY: Springer New York; 2013:465-482.
- Chandra C, Kachhal SK. Managing health care supply chain: trends, issues, and solutions from a logistics perspective. Paper presented at: Proceedings of the sixteenth annual society of health systems management engineering forum, February2004.
- Aston G. Supply chain. Teaming with physicians can drive down costs. Hospitals & health networks. 2010;84(1):13.
- Silver SA, Harel Z, McQuillan R, et al. How to begin a quality improvement project. Clinical Journal of the American Society of Nephrology. 2016;11(5):893-900.
- Sanford Health. Dedicated to the Work of Health and Healing. https://www.sanfordhealth.org/about. Published 2018. Accessed January 10, 2020.
- 11 Clinical Staff from Infection Prevention SCM, Quality, Education and Nursing, . In: Yapici HO, ed2019.
- Barry J, Allen C, Chlebeck M, Siebenaler R, Wick K, Gunderson W. Implementing a Two Person Insertion Technique and Indwelling Urinary Catheter Insertion Competency Assessment to Reduce Catheter Associated Urinary Tract Infections. American Journal of Infection Control. 2017;45(6):S60.
- Belizario SM. Preventing urinary tract infections with a two-person catheter insertion procedure. Nursing2019. 2015;45(3):67-69.
- Rhone C, Breiter Y, Benson L, Petri H, Thompson P, Murphy C. The impact of two-person indwelling urinary catheter insertion in the emergency department using technical and socioadaptive interventions. J Clin Outcomes Manag. 2017;24(10).
- Rebmann T, Greene LR. Preventing catheter-associated urinary tract infections: An executive summary of the Association for Professionals in Infection Control and Epidemiology, Inc, Elimination Guide. American Journal of Infection Control. 2010;38(8):644-646.
- Alexander JA, Hearld LR. Review: What Can We Learn From Quality Improvement Research?: A Critical Review of Research Methods. Medical Care Research and Review. 2009;66(3):235-271.
- Hovlid E, Bukve O, Haug K, Aslaksen AB, von Plessen C. Sustainability of healthcare improvement: what can we learn from learning theory? BMC Health Services Research. 2012;12(1):235.
- Kutney-Lee A, McHugh MD, Sloane DM, et al. Nursing: A Key To Patient Satisfaction. Health Affairs. 2009;28(4):w669-w677.
- Molyneux J. Nurses’ Job Satisfaction Linked to Patient Satisfaction. AJN The American Journal of Nursing. 2011;111(5):16.
- Perry SJ, Richter JP, Beauvais B. The Effects of Nursing Satisfaction and Turnover Cognitions on Patient Attitudes and Outcomes: A Three-Level Multisource Study. Health services research. 2018;53(6):4943-4969.