By Gina Thomas, RN, MBA, Lumere, Chief Development Officer
Cost = The amount that is paid to purchase something
This is an old topic that should be worn out. We have yet to conquer it.
Quality = An essential character of person, place, or thing
Quality isn’t just an effect of the function and features but how it’s used. In the case of healthcare, indications should be considered for the benefit to the patient.
I’m not going to belabor the point but let me mention a few trends that indicate fundamental problems with the current state of healthcare in the U.S.
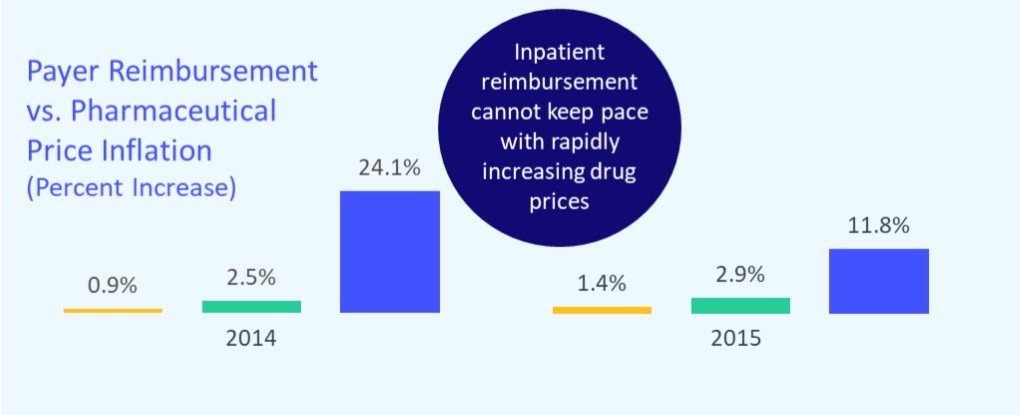
- Land of plenty – We have over 10,000 prescription drugs available to us in the US, which leads to a ‘this drug will cure all that ails you’ mentality. However, experts estimate that perhaps one-third of all US healthcare spending (COSTS) produces no benefit to the patient and some of it results in harm (QUALITY).
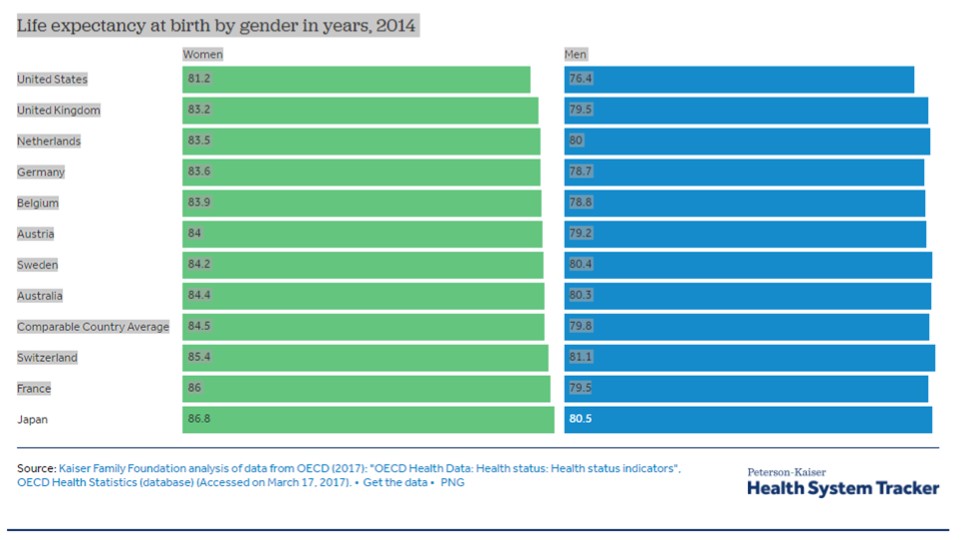
- While the US leads the world in healthcare costs, we do not come close to ranking high on quality of care. In fact, we rank poorly in life expectancy and other indicators of quality.
- While we know that higher intensity of care does improve outcomes, we spend a great deal more than other countries to achieve a similar degree of value. Examples of our higher costs include waste and variability in care that often lacks any evidence. Other countries don’t have nearly the resources or technology of the US, yet their value relative to the cost is markedly better.
Life expectancy for both men and women has increased slower in the U.S. than in comparable countries
Remember I wrote about Dr. Tower in my last article about the implant that he chose for his own hip replacement. The cost was not minimal and the poor outcomes demonstrate a lack of quality.
Our children will not be able to afford healthcare and the cycle will continue.
This is old news but it’s worth repeating. We can’t give up – we can’t forget—OUR LIVES DEPEND ON IT!
|
ACTION on Quality: |
|
· Review your processes to investigate quality compared to costs while asking yourself (and others) these questions to determine quality and value: |
|
|
|
ACTION on Costs: |
|

I will leave you with this last example of the interdependencies of cost and quality through a recent physician survey across multiple specialties:
90% of respondents felt increasing physician access to cost data would positively impact quality of care. Only 40% said their hospital or health system has measures that accurately capture quality of care for their specialties and patient population.
Look to MAKO in joint arthroplasty for a good example of cost and quality complexities around procedure types or patient populations.
Evidence indicates a lack of substantial improvement in clinical or operational outcomes and the extremely high capital and recurring cost associated with the MAKO robotic system. Its use in joint arthroplasty is likely not justified at this time. However, one flawed cost model suggests that use of the MAKO robotic system is cost-effective for unicompartmental knee arthroplasty at high-volume hospitals.
Patients want more also.
Patients are looking for more information on this topic as well and aren’t necessarily relying on websites like HospitalCompare or Healthgrades but turning to non-healthcare sites like Yelp.
“…But value—true consumer value—is not simply “quality minus cost.” (Or quality divided by cost…there seems to be a disagreement among academics about whether subtraction or division is more appropriate here.”) www.gisthealthcare.com/gist-blog
Quality and cost will always be tied together, and we shouldn’t accept anything less than a gold standard of high quality of health with longer age expectancy at a reasonable cost.
Gina Thomas, RN, MBA – As Lumere Chief Development Officer, Gina spearheads commercial strategies and helps guide product vision. With over 35 years of healthcare experience, starting as an emergency room nurse and later becoming a nursing executive, she brings a wealth of knowledge to the company, including strong expertise in preparing for new payment models, aligning clinicians, service line best practices, and executive-level approaches to resolving fragmentation in healthcare. She is passionate about patient advocacy. On a personal note, she has been married 32 years; has 2 daughters who she adores; and she says they have even found great guys who they married!
Sources:
Value-Based Payment Hits the Tipping Point. https://www.businesswire.com/news/home/20160613005067/en/Value-Based-Payment-Hits-Tipping-Point
Lumere Physician Study 2017
Morris M, Abrams K, Elsner N, Gerhardt W. Practicing Value-Based Care: What do doctors need? Deloitte. 2016.
Gisthealthcare.com
Robert Wood Johnson Foundation, “Reducing Overuse and Misuse: State Strategies to Improve Quality and Cost of Health Care,” January 2014.

